Angelika Amon, professor of biology and a member of the Koch Institute for Integrative Cancer Research, died on Oct. 29 at age 53, following a two-and-a-half-year battle with ovarian cancer.
“Known for her piercing scientific insight and infectious enthusiasm for the deepest questions of science, Professor Amon built an extraordinary career – and in the process, a devoted community of colleagues, students and friends,” MIT President L. Rafael Reif wrote in a letter to the MIT community.
“Angelika was a force of nature and a highly valued member of our community,” reflects Tyler Jacks, the David H. Koch Professor of Biology at MIT and director of the Koch Institute. “Her intellect and wit were equally sharp, and she brought unmatched passion to everything she did. Through her groundbreaking research, her mentorship of so many, her teaching, and a host of other contributions, Angelika has made an incredible impact on the world — one that will last long into the future.”
A pioneer in cell biology
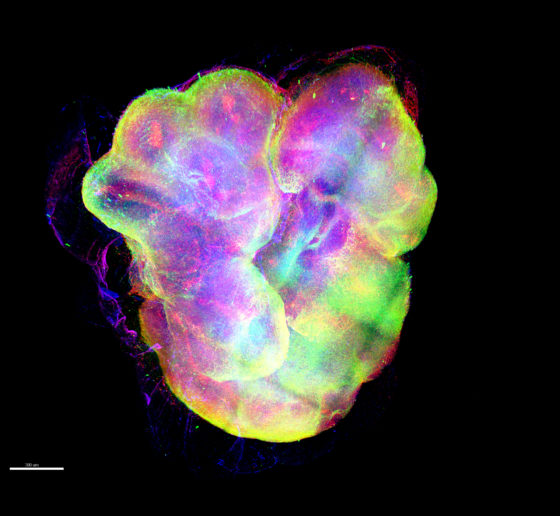
From the earliest stages of her career, Amon made profound contributions to our understanding of the fundamental biology of the cell, deciphering the regulatory networks that govern cell division and proliferation in yeast, mice, and mammalian organoids, and shedding light on the causes of chromosome mis-segregation and its consequences for human diseases.
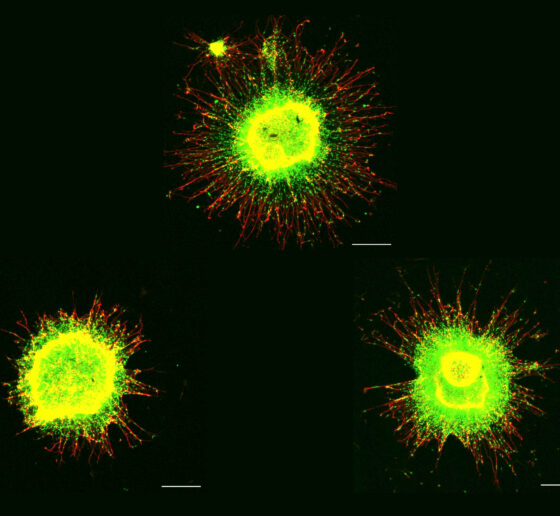
Human cells have 23 pairs of chromosomes, but as they divide they can make errors that lead to too many or too few chromosomes, resulting in aneuploidy. Amon’s meticulous and rigorous experiments, first in yeast and then in mammalian cells, helped to uncover the biological consequences of having too many chromosomes. Her studies determined that extra chromosomes significantly impact the composition of the cell, causing stress in important processes such as protein folding and metabolism, and leading to additional mistakes that could drive cancer. Although stress resulting from aneuploidy affects cells’ ability to survive and proliferate, cancer cells — which are nearly universally aneuploid — can grow uncontrollably. Amon showed that aneuploidy disrupts cells’ usual error-repair systems, allowing genetic mutations to quickly accumulate.
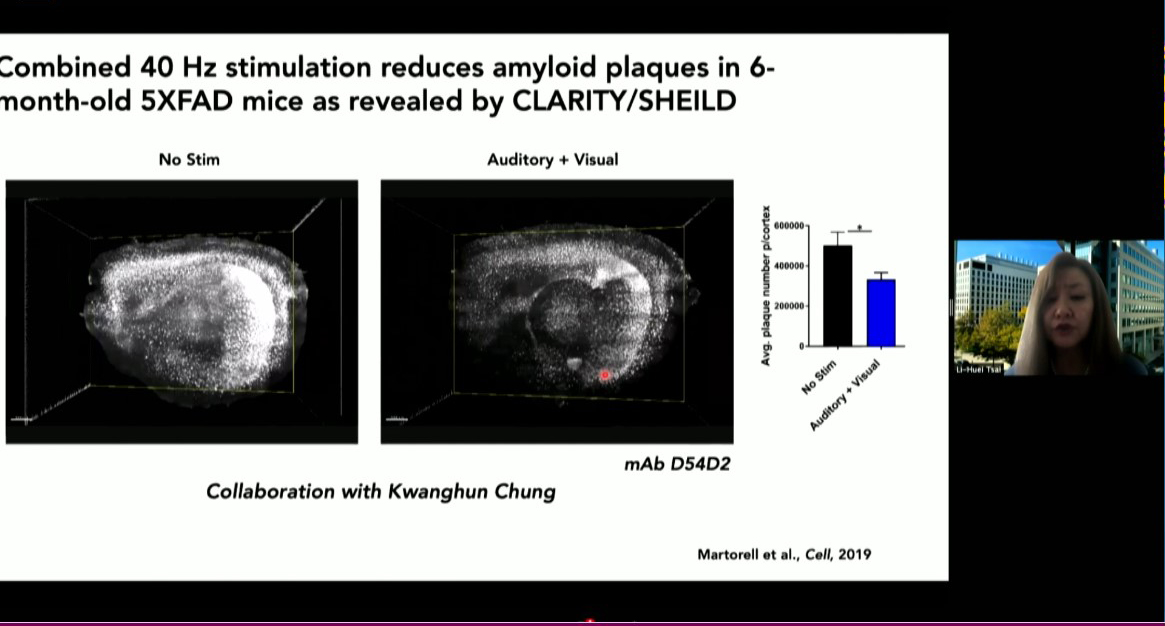
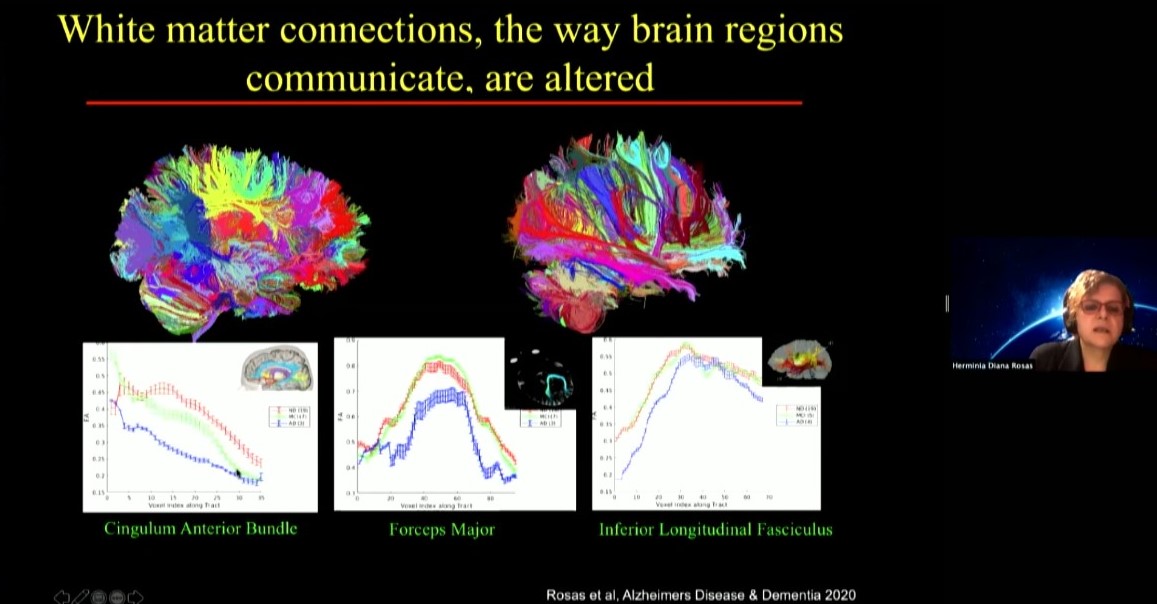
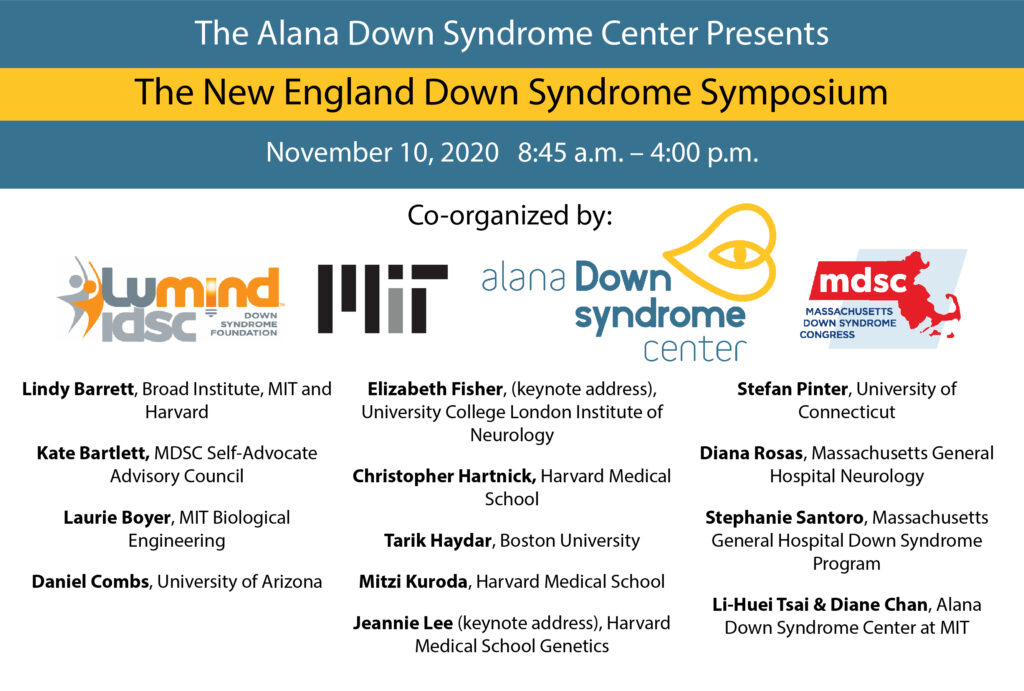
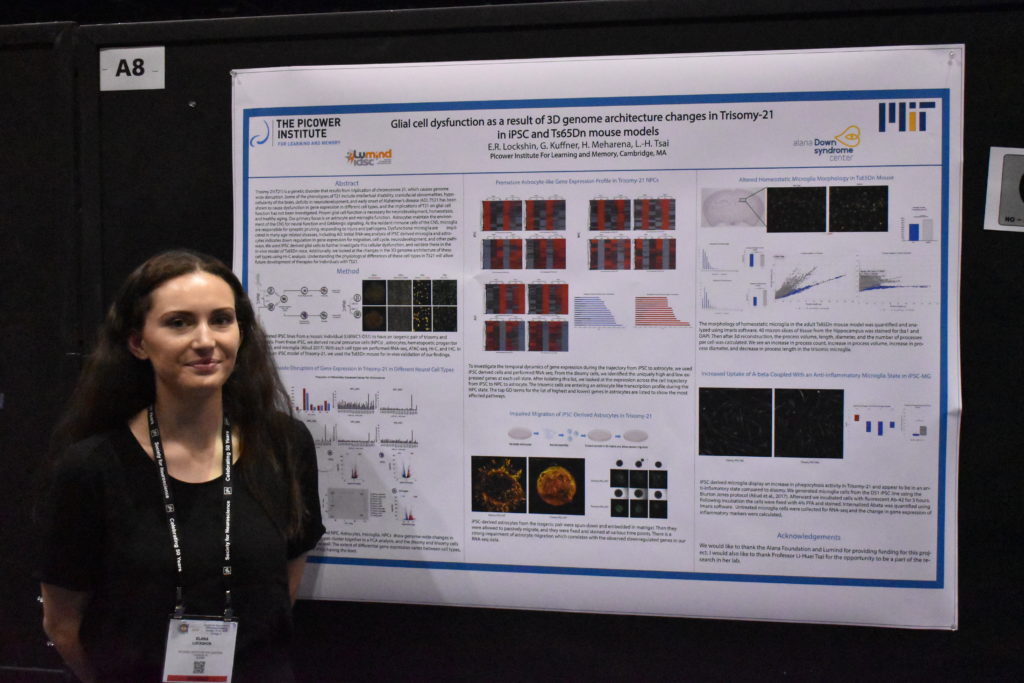
Aneuploidy is usually fatal, but in some instances extra copies of specific chromosomes can lead to conditions such as Down syndrome and developmental disorders including those known as Patau and Edwards syndromes. This led Amon to work to understand how these negative effects result in some of the health problems associated specifically with Down syndrome, such as acute lymphoblastic leukemia. Her expertise in this area led her to be named co-director of the recently established Alana Down Syndrome Center at MIT.
“Angelika’s intellect and research were as astonishing as her bravery and her spirit. Her lab’s fundamental work on aneuploidy was integral to our establishment of the center,” say Li-Huei Tsai, the Picower Professor of Neuroscience and co-director of the Alana Down Syndrome Center. “Her exploration of the myriad consequences of aneuploidy for human health was vitally important and will continue to guide scientific and medical research.”
Another major focus of research in the Amon lab has been on the relationship between how cells grow, divide, and age. Among other insights, this work has revealed that once cells reach a certain large size, they lose the ability to proliferate and are unable to reenter the cell cycle. Further, this growth contributes to senescence, an irreversible cell cycle arrest, and tissue aging. In related work, Amon has investigated the relationships between stem cell size, stem cell function, and tissue age. Her lab’s studies have found that in hematopoetic stem cells, small size is important to cells’ ability to function and proliferate — in fact, she posted recent findings on bioRxiv earlier this week — and have been examining the same questions in epithelial cells as well.
Amon lab experiments delved deep into the mechanics of the biology, trying to understand the mechanisms behind their observations. To support this work, she established research collaborations to leverage approaches and technologies developed by her colleagues at the Koch Institute, including sophisticated intestinal organoid and mouse models developed by the Yilmaz Laboratory, and a microfluidic device developed by the Manalis Laboratory for measuring physical characteristics of single cells.
The thrill of discovery
Born in 1967, Amon grew up in Vienna, Austria, in a family of six. Playing outside all day with her three younger siblings, she developed an early love of biology and animals. She could not remember a time when she was not interested in biology, initially wanting to become a zoologist. But in high school, she saw an old black-and-white film from the 1950s about chromosome segregation, and found the moment that the sister chromatids split apart breathtaking. She knew then that she wanted to study the inner workings of the cell and decided to focus on genetics at the University of Vienna in Austria.
After receiving her BS, Amon continued her doctoral work there under Professor Kim Nasmyth at the Research Institute of Molecular Pathology, earning her PhD in 1993. From the outset, she made important contributions to the field of cell cycle dynamics. Her work on yeast genetics in the Nasmyth laboratory led to major discoveries about how one stage of the cell cycle sets up for the next, revealing that cyclins, proteins that accumulate within cells as they enter mitosis, must be broken down before cells pass from mitosis to G1, a period of cell growth.
Towards the end of her doctorate, Amon became interested in fruitfly genetics and read the work of Ruth Lehmann, then a faculty member at MIT and a member of the Whitehead Institute. Impressed by the elegance of Lehmann’s genetic approach, she applied and was accepted to her lab. In 1994, Amon arrived in the United States, not knowing that it would become her permanent home or that she would eventually become a professor.
While Amon’s love affair with fruitfly genetics would prove short, her promise was immediately apparent to Lehmann, now director of the Whitehead Institute. “I will never forget picking Angelika up from the airport when she was flying in from Vienna to join my lab. Despite the long trip, she was just so full of energy, ready to talk science,” says Lehmann. “She had read all the papers in the new field and cut through the results to hit equally on the main points.”
But as Amon frequently was fond of saying, “yeast will spoil you.” Lehmann explains that “because they grow so fast and there are so many tools, ‘your brain is the only limitation.’ I tried to convince her of the beauty and advantages of my slower-growing favorite organism. But in the end, yeast won and Angelika went on to establish a remarkable body of work, starting with her many contributions to how cells divide and more recently to discover a cellular aneuploidy program.”
In 1996, after Lehmann had left for New York University’s Skirball Institute, Amon was invited to become a Whitehead Fellow, a prestigious program that offers recent PhDs resources and mentorship to undertake their own investigations. Her work on the question of how yeast cells progress through the cell cycle and partition their chromosomes would be instrumental in establishing her as one of the world’s leading geneticists. While at Whitehead, her lab made key findings centered around the role of an enzyme called Cdc14 in prompting cells to exit mitosis, including that the enzyme is sequestered in a cellular compartment called the nucleolus and must be released before the cell can exit.
“I was one of those blessed to share with her a ‘eureka moment,’ as she would call it,” says Rosella Visintin, a postdoc in Amon’s lab at the time of the discovery and now an assistant professor at the European School of Molecular Medicine in Milan. “She had so many. Most of us are lucky to get just one, and I was one of the lucky ones. I’ll never forget her smile and scream — neither will the entire Whitehead Institute — when she saw for the first time Cdc14 localization: ‘You did it, you did it, you figured it out!’ Passion, excitement, joy — everything was in that scream.”
In 1999, Amon’s work as a Whitehead Fellow earned her a faculty position in the MIT Department of Biology and the MIT Center for Cancer Research, the predecessor to the Koch Institute. A full professor since 2007, she also became the Kathleen and Curtis Marble Professor in Cancer Research, associate director of the Paul F. Glenn Center for Biology of Aging Research at MIT, a member of the Ludwig Center for Molecular Oncology at MIT, and an investigator of the Howard Hughes Medical Institute.
Her pathbreaking research was recognized by several awards and honors, including the 2003 National Science Foundation Alan T. Waterman Award, the 2007 Paul Marks Prize for Cancer Research, the 2008 National Academy of Sciences (NAS) Award in Molecular Biology, and the 2013 Ernst Jung Prize for Medicine. In 2019, she won the Breakthrough Prize in Life Sciences and the Vilcek Prize in Biomedical Science, and was named to the Carnegie Corporation of New York’s annual list of Great Immigrants, Great Americans. This year, she was given the Human Frontier Science Program Nakasone Award. She was also a member of the NAS and the American Academy of Arts and Sciences.
Lighting the way forward
Amon’s perseverance, deep curiosity, and enthusiasm for discovery served her well in her roles as teacher, mentor, and colleague. She has worked with many labs across the world and developed a deep network of scientific collaboration and friendships. She was a sought-after speaker for seminars and the many conferences she attended. In over 20 years as a professor at MIT, she has mentored more than 80 postdocs, graduate students, and undergraduates, and received the School of Science’s undergraduate teaching prize.
“Angelika was an amazing, energetic, passionate, and creative scientist, an outstanding mentor to many, and an excellent teacher,” says Alan Grossman, the Praecis Professor of Biology and head of MIT’s Department of Biology. “Her impact and legacy will live on and be perpetuated by all those she touched.”
“Angelika existed in a league of her own,” explains Kristin Knouse, one of Amon’s former graduate students and a current Whitehead Fellow. “She had the energy and excitement of someone who picked up a pipette for the first time, but the brilliance and wisdom of someone who had been doing it for decades. Her infectious energy and brilliant mind were matched by a boundless heart and tenacious grit. She could glance at any data and immediately deliver a sharp insight that would never have crossed any other mind. Her positive attributes were infectious, and any interaction with her, no matter how transient, assuredly left you feeling better about yourself and your science.”
Taking great delight in helping young scientists find their own “eureka moments,” Amon was a fearless advocate for science and the rights of women and minorities and inspired others to fight as well. She was not afraid to speak out in support of the research and causes she believed strongly in. She was a role model for young female scientists and spent countless hours mentoring and guiding them in a male-dominated field. While she graciously accepted awards for women in science, including the Vanderbilt Prize and the Women in Cell Biology Senior Award, she questioned the value of prizes focused on women as women, rather than on their scientific contributions.
“Angelika Amon was an inspiring leader,” notes Lehmann, “not only by her trailblazing science but also by her fearlessness to call out sexism and other -isms in our community. Her captivating laugh and unwavering mentorship and guidance will be missed by students and faculty alike. MIT and the science community have lost an exemplary leader, mentor, friend, and mensch.”
Amon’s wide-ranging curiosity led her to consider new ideas beyond her own field. In recent years, she has developed a love for dinosaurs and fossils, and often mentioned that she would like to study terraforming, which she considered essential for a human success to life on other planets.
“It was always amazing to talk with Angelika about science, because her interests were so deep and so broad, her intellect so sharp, and her enthusiasm so infectious,” remembers Vivian Siegel, a lecturer in the Department of Biology and friend since Amon’s postdoctoral days. “Beyond her own work in the lab, she was fascinated by so many things, including dinosaurs — dreaming of taking her daughters on a dig — lichen, and even life on Mars.”
“Angelika was brilliant; she illuminated science and scientists,” says Frank Solomon, professor of biology and member of the Koch Institute. “And she was intense; she warmed the people around her, and expanded what it means to be a friend.”
Amon is survived by her husband Johannes Weis, and her daughters Theresa and Clara Weis, and her three siblings and their families.
–From MIT News