In Brisbane, Australia, the World Down Syndrome Congress convened in-person for the first time since 2018. Over 1000 delegates from 45 countries met from July 9th – 12th, 2024, for the central theme of “Together We Can: Celebrating Diversity and Inclusion.” The event allowed families, advocates and professionals from the global Down syndrome community to gather and discuss all aspects of health, research, education, employment, inclusion and personal development. The Alana Down Syndrome Center (ADSC) of MIT was honored to be featured in a plenary session focused on the center’s ongoing research supported by the Alana Foundation.
The session, chaired by Professor Rhonda Faragher, was not a typical scientific meeting, as it included self-advocates and families as participants in the discussion. Panelists included Jaspreet Kaur Sekhon from Singapore who has overcome adversity as a leading self-advocate for Down syndrome. Her long list of accolades includes a keynote presentation at the United Nations, and decades of dance performance and instruction for young people with disabilities. Jessamy Tang, MIT graduate and Managing Director of the Stanford Down Syndrome Research Center, and Nathan Rowe, Program Director at Down Syndrome International, rounded out the panel with their deep expertise in disability inclusion.
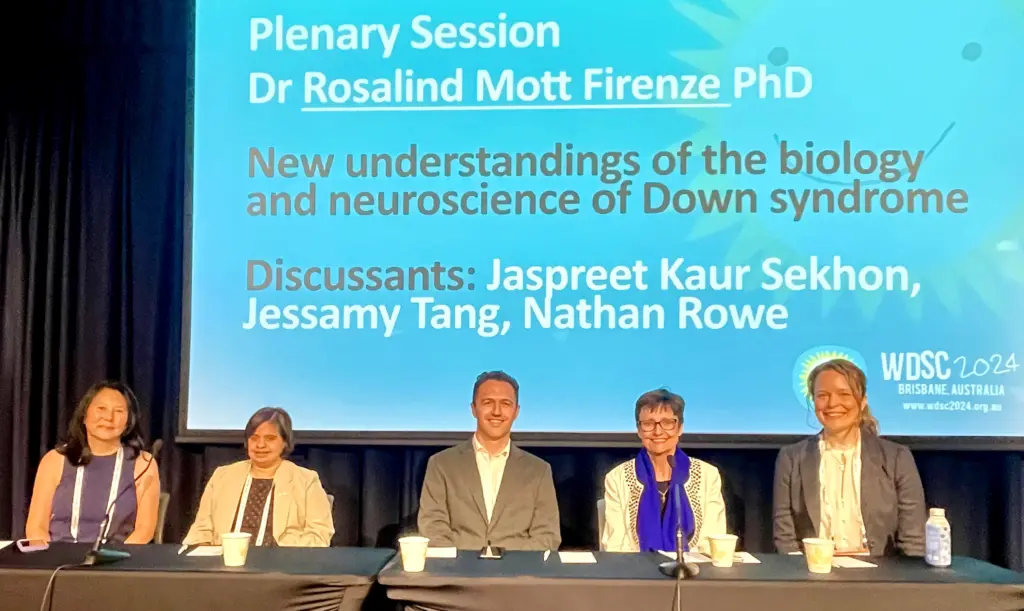
The program director of ADSC, Dr. Rosalind Firenze, featured the work of the center and highlighted the recent clinical study, led by Dr. Diane Chan and Picower Professor Li-Huei Tsai, Director of the ADSC and The Picower Institute for Learning and Memory of MIT. Tsai’s group is developing a ground-breaking, non-invasive therapy for Alzheimer’s disease known as ‘GENUS’ – gamma entrainment through non-invasive 40Hz sensory stimulation. The landmark clinical trial, the first to study the effects of GENUS in people with Down syndrome, was recently completed at MIT. The results are currently being analyzed with initial outcomes indicating that light and sound stimulation can increase the strength of 40Hz gamma rhythms in the brain and may provide cognitive benefits in the short-term. Long-term studies in people with Down syndrome and Alzheimer’s disease are still needed to test the therapeutic efficacy of this non-invasive approach.
Firenze also highlighted another MIT invention: ZzAlign, which is a comfortable, mouth-piece device under development to help people with obstructive sleep apnea (OSA) keep airways open. The new device incorporates digital intraoral scans, 3D printing technology and an innovative smart-pump design to apply a gentle suction pressure to hold the tongue in place, effectively opening airways during sleep. OSA impacts the majority of adults with Down syndrome and impacts their overall health. The development of ZzAlign is led by Professor Ellen Roche‘s lab and the Deshpande Center for Technological Innovation. The team is currently entering clinical trials to test the device’s efficacy during sleep in people with OSA.
Families and self-advocates learned about other ADSC research, including the use of iPSC (induced pluripotent stem cell) models to study changes in heart development and application of GENUS to improve neurodevelopment in the T65Dn mouse model of Down syndrome. After learning about the research tools and progress, audience members participated in an engaging discussion on the role of scientific research in attaining a higher quality of life for people with Down syndrome. Sekhon pointed out the importance of including self-advocates in research design and discussions to ensure that their needs are considered and incorporated. Tang further championed the concept of consulting with families in the early stages of clinical trial design to ensure that participation is accessible and comfortable. Rowe also pointed out that once technologies and therapies are developed it is important to make them available in a fair and equitable way. Audience members asked questions about how the model systems relate back to people with Down syndrome and when therapies like GENUS might become available.
By connecting the Down syndrome community directly to cutting-edge research at MIT, the plenary session felt momentous with an important take-away: inclusivity can push science further. Jaspreet Kaur Sekhon said it best herself, as she thanked researchers at ADSC and the panel, “You all were very inclusive, in giving me this Voice and listening to me.”



