Tag: People
Angelika Amon, research pioneer and ADSC founding member, dies at 53

MIT is mourning the passing of biologist Angelika Amon, co-director of the Alana Down Syndrome Center. She died of cancer after living with the disease for two-and-a-half years. “Angelika’s intellect and research were as astonishing as her bravery and her spirit,” said her Alana colleague Li-Huei Tsai.
Angelika Amon, professor of biology and a member of the Koch Institute for Integrative Cancer Research, died on Oct. 29 at age 53, following a two-and-a-half-year battle with ovarian cancer.
“Known for her piercing scientific insight and infectious enthusiasm for the deepest questions of science, Professor Amon built an extraordinary career – and in the process, a devoted community of colleagues, students and friends,” MIT President L. Rafael Reif wrote in a letter to the MIT community.
“Angelika was a force of nature and a highly valued member of our community,” reflects Tyler Jacks, the David H. Koch Professor of Biology at MIT and director of the Koch Institute. “Her intellect and wit were equally sharp, and she brought unmatched passion to everything she did. Through her groundbreaking research, her mentorship of so many, her teaching, and a host of other contributions, Angelika has made an incredible impact on the world — one that will last long into the future.”
A pioneer in cell biology
From the earliest stages of her career, Amon made profound contributions to our understanding of the fundamental biology of the cell, deciphering the regulatory networks that govern cell division and proliferation in yeast, mice, and mammalian organoids, and shedding light on the causes of chromosome mis-segregation and its consequences for human diseases.
Human cells have 23 pairs of chromosomes, but as they divide they can make errors that lead to too many or too few chromosomes, resulting in aneuploidy. Amon’s meticulous and rigorous experiments, first in yeast and then in mammalian cells, helped to uncover the biological consequences of having too many chromosomes. Her studies determined that extra chromosomes significantly impact the composition of the cell, causing stress in important processes such as protein folding and metabolism, and leading to additional mistakes that could drive cancer. Although stress resulting from aneuploidy affects cells’ ability to survive and proliferate, cancer cells — which are nearly universally aneuploid — can grow uncontrollably. Amon showed that aneuploidy disrupts cells’ usual error-repair systems, allowing genetic mutations to quickly accumulate.
Aneuploidy is usually fatal, but in some instances extra copies of specific chromosomes can lead to conditions such as Down syndrome and developmental disorders including those known as Patau and Edwards syndromes. This led Amon to work to understand how these negative effects result in some of the health problems associated specifically with Down syndrome, such as acute lymphoblastic leukemia. Her expertise in this area led her to be named co-director of the recently established Alana Down Syndrome Center at MIT.
“Angelika’s intellect and research were as astonishing as her bravery and her spirit. Her lab’s fundamental work on aneuploidy was integral to our establishment of the center,” say Li-Huei Tsai, the Picower Professor of Neuroscience and co-director of the Alana Down Syndrome Center. “Her exploration of the myriad consequences of aneuploidy for human health was vitally important and will continue to guide scientific and medical research.”
Another major focus of research in the Amon lab has been on the relationship between how cells grow, divide, and age. Among other insights, this work has revealed that once cells reach a certain large size, they lose the ability to proliferate and are unable to reenter the cell cycle. Further, this growth contributes to senescence, an irreversible cell cycle arrest, and tissue aging. In related work, Amon has investigated the relationships between stem cell size, stem cell function, and tissue age. Her lab’s studies have found that in hematopoetic stem cells, small size is important to cells’ ability to function and proliferate — in fact, she posted recent findings on bioRxiv earlier this week — and have been examining the same questions in epithelial cells as well.
Amon lab experiments delved deep into the mechanics of the biology, trying to understand the mechanisms behind their observations. To support this work, she established research collaborations to leverage approaches and technologies developed by her colleagues at the Koch Institute, including sophisticated intestinal organoid and mouse models developed by the Yilmaz Laboratory, and a microfluidic device developed by the Manalis Laboratory for measuring physical characteristics of single cells.
The thrill of discovery
Born in 1967, Amon grew up in Vienna, Austria, in a family of six. Playing outside all day with her three younger siblings, she developed an early love of biology and animals. She could not remember a time when she was not interested in biology, initially wanting to become a zoologist. But in high school, she saw an old black-and-white film from the 1950s about chromosome segregation, and found the moment that the sister chromatids split apart breathtaking. She knew then that she wanted to study the inner workings of the cell and decided to focus on genetics at the University of Vienna in Austria.
After receiving her BS, Amon continued her doctoral work there under Professor Kim Nasmyth at the Research Institute of Molecular Pathology, earning her PhD in 1993. From the outset, she made important contributions to the field of cell cycle dynamics. Her work on yeast genetics in the Nasmyth laboratory led to major discoveries about how one stage of the cell cycle sets up for the next, revealing that cyclins, proteins that accumulate within cells as they enter mitosis, must be broken down before cells pass from mitosis to G1, a period of cell growth.
Towards the end of her doctorate, Amon became interested in fruitfly genetics and read the work of Ruth Lehmann, then a faculty member at MIT and a member of the Whitehead Institute. Impressed by the elegance of Lehmann’s genetic approach, she applied and was accepted to her lab. In 1994, Amon arrived in the United States, not knowing that it would become her permanent home or that she would eventually become a professor.
While Amon’s love affair with fruitfly genetics would prove short, her promise was immediately apparent to Lehmann, now director of the Whitehead Institute. “I will never forget picking Angelika up from the airport when she was flying in from Vienna to join my lab. Despite the long trip, she was just so full of energy, ready to talk science,” says Lehmann. “She had read all the papers in the new field and cut through the results to hit equally on the main points.”
But as Amon frequently was fond of saying, “yeast will spoil you.” Lehmann explains that “because they grow so fast and there are so many tools, ‘your brain is the only limitation.’ I tried to convince her of the beauty and advantages of my slower-growing favorite organism. But in the end, yeast won and Angelika went on to establish a remarkable body of work, starting with her many contributions to how cells divide and more recently to discover a cellular aneuploidy program.”
In 1996, after Lehmann had left for New York University’s Skirball Institute, Amon was invited to become a Whitehead Fellow, a prestigious program that offers recent PhDs resources and mentorship to undertake their own investigations. Her work on the question of how yeast cells progress through the cell cycle and partition their chromosomes would be instrumental in establishing her as one of the world’s leading geneticists. While at Whitehead, her lab made key findings centered around the role of an enzyme called Cdc14 in prompting cells to exit mitosis, including that the enzyme is sequestered in a cellular compartment called the nucleolus and must be released before the cell can exit.
“I was one of those blessed to share with her a ‘eureka moment,’ as she would call it,” says Rosella Visintin, a postdoc in Amon’s lab at the time of the discovery and now an assistant professor at the European School of Molecular Medicine in Milan. “She had so many. Most of us are lucky to get just one, and I was one of the lucky ones. I’ll never forget her smile and scream — neither will the entire Whitehead Institute — when she saw for the first time Cdc14 localization: ‘You did it, you did it, you figured it out!’ Passion, excitement, joy — everything was in that scream.”
In 1999, Amon’s work as a Whitehead Fellow earned her a faculty position in the MIT Department of Biology and the MIT Center for Cancer Research, the predecessor to the Koch Institute. A full professor since 2007, she also became the Kathleen and Curtis Marble Professor in Cancer Research, associate director of the Paul F. Glenn Center for Biology of Aging Research at MIT, a member of the Ludwig Center for Molecular Oncology at MIT, and an investigator of the Howard Hughes Medical Institute.
Her pathbreaking research was recognized by several awards and honors, including the 2003 National Science Foundation Alan T. Waterman Award, the 2007 Paul Marks Prize for Cancer Research, the 2008 National Academy of Sciences (NAS) Award in Molecular Biology, and the 2013 Ernst Jung Prize for Medicine. In 2019, she won the Breakthrough Prize in Life Sciences and the Vilcek Prize in Biomedical Science, and was named to the Carnegie Corporation of New York’s annual list of Great Immigrants, Great Americans. This year, she was given the Human Frontier Science Program Nakasone Award. She was also a member of the NAS and the American Academy of Arts and Sciences.
Lighting the way forward
Amon’s perseverance, deep curiosity, and enthusiasm for discovery served her well in her roles as teacher, mentor, and colleague. She has worked with many labs across the world and developed a deep network of scientific collaboration and friendships. She was a sought-after speaker for seminars and the many conferences she attended. In over 20 years as a professor at MIT, she has mentored more than 80 postdocs, graduate students, and undergraduates, and received the School of Science’s undergraduate teaching prize.
“Angelika was an amazing, energetic, passionate, and creative scientist, an outstanding mentor to many, and an excellent teacher,” says Alan Grossman, the Praecis Professor of Biology and head of MIT’s Department of Biology. “Her impact and legacy will live on and be perpetuated by all those she touched.”
“Angelika existed in a league of her own,” explains Kristin Knouse, one of Amon’s former graduate students and a current Whitehead Fellow. “She had the energy and excitement of someone who picked up a pipette for the first time, but the brilliance and wisdom of someone who had been doing it for decades. Her infectious energy and brilliant mind were matched by a boundless heart and tenacious grit. She could glance at any data and immediately deliver a sharp insight that would never have crossed any other mind. Her positive attributes were infectious, and any interaction with her, no matter how transient, assuredly left you feeling better about yourself and your science.”
Taking great delight in helping young scientists find their own “eureka moments,” Amon was a fearless advocate for science and the rights of women and minorities and inspired others to fight as well. She was not afraid to speak out in support of the research and causes she believed strongly in. She was a role model for young female scientists and spent countless hours mentoring and guiding them in a male-dominated field. While she graciously accepted awards for women in science, including the Vanderbilt Prize and the Women in Cell Biology Senior Award, she questioned the value of prizes focused on women as women, rather than on their scientific contributions.
“Angelika Amon was an inspiring leader,” notes Lehmann, “not only by her trailblazing science but also by her fearlessness to call out sexism and other -isms in our community. Her captivating laugh and unwavering mentorship and guidance will be missed by students and faculty alike. MIT and the science community have lost an exemplary leader, mentor, friend, and mensch.”
Amon’s wide-ranging curiosity led her to consider new ideas beyond her own field. In recent years, she has developed a love for dinosaurs and fossils, and often mentioned that she would like to study terraforming, which she considered essential for a human success to life on other planets.
“It was always amazing to talk with Angelika about science, because her interests were so deep and so broad, her intellect so sharp, and her enthusiasm so infectious,” remembers Vivian Siegel, a lecturer in the Department of Biology and friend since Amon’s postdoctoral days. “Beyond her own work in the lab, she was fascinated by so many things, including dinosaurs — dreaming of taking her daughters on a dig — lichen, and even life on Mars.”
“Angelika was brilliant; she illuminated science and scientists,” says Frank Solomon, professor of biology and member of the Koch Institute. “And she was intense; she warmed the people around her, and expanded what it means to be a friend.”
Amon is survived by her husband Johannes Weis, and her daughters Theresa and Clara Weis, and her three siblings and their families.
Down Syndrome symposium presents bench-to-bedside research

At its first ever symposium Nov. 6, the Alana Down Syndrome Center demonstrated ways, from the scale of chromosomes to that of caregiving communities, that scientists and physicians in Massachusetts and around the country are working to help people with Down syndrome live their healthiest, fullest lives.
Founded at MIT in March 2019, the ADSC brings together neuroscience, biology, engineering and computer science research labs together with the Desphande Center for Technological Innovation to deepen knowledge about Down syndrome and to improve health, autonomy and inclusion of people with the genetic condition characterized by an extra copy of chromosome 21.
The symposium, “Translational Research in Down Syndrome,” brought together experts working across a spectrum of fundamental biology to clinical care. In her opening remarks, ADSC co-director Li-Huei Tsai, Picower Professor of Neuroscience and director of The Picower Institute for Learning and Memory, said the event represented a chance for conversation and collaboration among researchers with the common goal of helping people with Down syndrome.
“Informed and inspired by their remarks we can all engage today in learning from each other,” she said. Tsai also thanked Ana Lucia Villela, whose Alana Foundation gift established the center and who had returned to MIT from Brazil to attend the symposium.
‘Aneuploidy’ advances
Throughout the afternoon, speakers shared some of their latest insights into how “aneuploidy,” having an atypical number of chromosomes, alters the biology of cells, the body and the brain.
One consequence appears to be that with an extra chromosome, cells make too many copies of the protein subunits that the chromosome encodes. Normally these subunits would become bound with partners encoded elsewhere into larger protein complexes, said ADSC Co-Director Angelika Amon, Kathleen and Curtis Marble Professor of Cancer Research in MIT’s biology department and the Koch Center for Integrative Cancer Research. But there aren’t as many of those partners, so the excess, unbound proteins become prone to clumping together, creating a major clean-up job for the cells that causes ”proteotoxic” stress. In Down syndrome, she said, that stress can hinder growth and proper function. Aneuploidy, she added, might also lead to a greater incidence of DNA damage.

Former Amon lab postdoc Eduardo Torres, who is now at the University of Massachusetts Medical School, said his lab has found that aneuploidy also disrupts the very shape and structure of the nucleus in a variety of cells, making them more sensitive to mechanical stress. The lab looked deeper to find the genetic and molecular pathway responsible and identified one related to the lipid composition of the nucleus. That insight allowed them to discover that administering certain drugs to cells with aneuploidy of chromosome 21 (or 13 or 18) can help shore up the nuclear structure and help cells grow.
To gain more insight into how aneuploidy affects neurological development many scientists have begun using techniques to grow brain cells from stem cells derived from Down syndrome patients. They can manipulate these cultures in the lab so that the only genetic difference is the extra copy of chromosome 21. Jeanne Lawrence, also of UMass, said use of such advanced models will help her understand whether a technique her lab has developed to silence extra copies of a chromosome will be effective in cells such as those in the brain or blood. Her work shows promise for a potential gene therapy to mitigate the effects of the extra copy of chromosome 21.
Another vital model of Down syndrome is the mouse. In one of the day’s two keynote addresses, Roger Reeves of the McKusick-Nathans Institute for Genetic Medicine at Johns Hopkins University described what researchers have learned from the widely used T65dn mouse model, as well as what they hope to learn from a newly developed model, that uses human chromosome 21 genes to replicate chromosome duplication. He also described their studies of the developmental anomalies in Down syndrome model mouse brains, and have found that a crucial signaling pathway for development is less responsive in these mice. He reported the results of a screen to look for the specific contributors this pathway in DS, as they may be viable targets for drug development, and his lab has also identified some of these same genes to be involved in congenital heart defects.
Clinical care
In the symposium’s other keynote, Joaquin Espinosa of the Linda Crnic Institute for Down Syndrome at the University of Colorado, discussed how a fast-emerging raft of insights including discoveries about the immune system in Down syndrome has led to a new clinical trial. Fundamental research at the institute has found that patients with Down syndrome have an increased sensitivity to interferons, proteins emitted by immune cells as they fight infections. The research led scientists to test medicines to calm the immune system. He described their current work on a clinical trial that aims to investigate a drug, Xeljanz, already used for auto-immune disease, to see if the drug not only improves autoimmune skin diseases, but possibly a wider range of symptoms associated with Down syndrome.
Another clinical trial is getting underway at Boston Children’s Hospital, said Nicole Baumer, a researcher there who said there are real opportunities for interventions to improve cognition in Down syndrome patients, but who also cautioned that researchers must always consult patients and their caregivers about what they want from clinical trials and care, rather than assuming what’s best for them. After surveying to learn more about patient and family wishes, her group has designed a study in which they will try to predict the neurodevelopmental outcomes in babies with Down syndrome, and test whether behavioral therapy interventions designed for certain autism populations might also augment intellectual development in children with Down syndrome.

As researchers strive in the lab and clinic to make new discoveries and improve care, Brian Skotko of Massachusetts General Hospital and Harvard Medical School has also been considering how to ensure that state-of-the-art information reaches doctors and family caregivers everywhere it’s needed. Skotko noted that among approximately 212,000 people with Down syndrome in the United States, less than five percent have access to one of the 71 specialty clinics around the country like the one he directs at MGH. Instead, they typically depend on primary care physicians. That’s why he and a diverse team have spent the last two years developing an Internet-based platform, “Down Syndrome Clinic to You (DSC2U)” in which a physician or other caregiver can enter information about a patient and learn richly linked, expert-curated information and recommendations about medical care and wellness customized for the entered patient profile. The clinical team at MGH reviews the underlying database regularly to keep it up to date. With new data showing that the system positively influences care and has been valued by users, it’s ready for a wider launch next year, he said.
Taken together, the symposium talks illustrated many routes to potential progress, from the cell to the clinic.
ADSC researchers at Society for Neuroscience 2019
Special Lecture by ADSC co-Director Dr. Li-Huei Tsai
“Leveraging Brain Rhythms as a Therapeutic Intervention for Neurodegenerative Diseases”
Session 443: Oct 22, 12 – 1:10pm, Hall B
Posters
Oct 20:
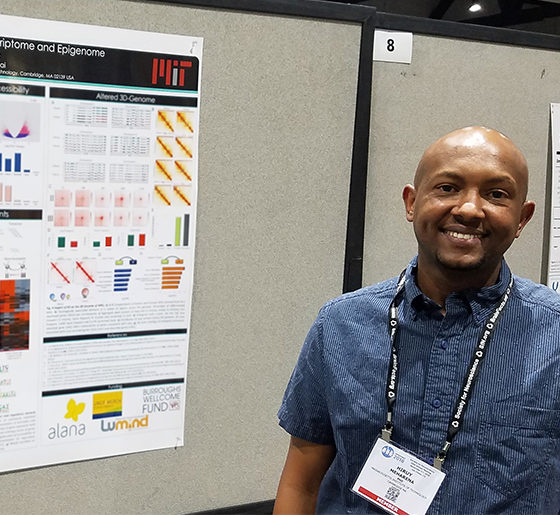
| Hiruy Meharena | Tsai lab |
Altered 3D-Genome Architecture of Neural Progenitor Cells as a Consequence of Down Syndrome |
Session 113.26 8 AM- 12 PM |
Oct 21:
| Y.-T. Lin | Tsai lab |
Engineered human cerebral organoids as a model for studying Down Syndrome |
Session 278.19 8 AM- 12 PM |
Oct 22:
| C. Addaikkan | Tsai lab |
Identifying neural circuits underlying visually evoked entrainment |
Session 577.08 1 PM- 5 PM |
| A. Payne | Boyden lab |
Genome-wide in situ sequencing |
Session 611.05 1 PM- 5 PM |
| A. Sinha | Boyden lab |
Targeted and untargeted in situ sequencing in thick, physically magnified brain tissue |
Session 611.06 1 PM- 5 PM |
Oct 23:
| E.R. Lockshin | Tsai lab |
Glial cell dysfunction as a result of 3D genome architecture changes in risomy-21 iPSC and ts65DN mouse models |
Session 729.08 1 PM- 5 PM |
| B. Jackson | Tsai & Boyden labs |
Extended gamma sensory stimulation in cognitively normal individuals |
Session 771.06 1 PM- 5 PM |
| D. Sarkar | Boyden lab |
Iterative direct expansion microscopy |
Session 794.08 1 PM- 5 PM |
Blending complementary expertise, Tsai and Kellis labs tackle brain diseases

Li-Huei Tsai is a neuroscientist and Manolis Kellis is a computer scientist, so by working together, their research teams are able to ask questions about the big data of the brain that neither one could alone.
In their collaboration to help elucidate and mitigate Alzheimer’s disease and other neurological conditions, the labs of neuroscientist Li-Huei Tsai and computer scientist Manolis Kellis are two sides of the same coin on two sides of Vassar Street.
Bringing complementary skills to a shared mission as part of MIT’s Aging Brain Initiative and Alana Down Syndrome Center, the team seamlessly blends and advances some of the hottest and most powerful methods in science – statistical genetics, computational genomics, epigenomics, machine learning, single-cell profiling, “big data” integration, induced stem-cell reprogramming, mini-brain organoids, tissue engineering, and CRISPR-Cas9 genetic manipulation.This allows their teams to study genetic and molecular differences between healthy and diseased samples from multiple brain regions of humans and mice, integrate and analyze the resulting data to identify significant disease-driver genes and the cell types where they act, and engineer cells, tissues and mouse models to test their hypotheses and discover therapeutic interventions.
“Working together, we have the opportunity to garner big data from a large number of human subjects to elucidate the driver genes and pathways that are novel but key to the disease,” said Tsai, Picower Professor and director of the Picower Institute for Learning and Memory. “We can then test these genes/pathways in the induced pluripotent stem cells (iPSC) system coupled with CRISPR-Cas9 to manipulate the genome. We can induce the iPS cells into all major brain cell types, and dissect the contributions of each of these cell types to disease.”
It’s a joint research venture that’s as close, cutting-edge, and multidisciplinary as any at MIT, and fits squarely within the Schwarzman College of Computing’s emphasis on integrating artificial intelligence with the sciences. Kellis recalls it all getting started back in 2012 via the connection of postdocs, Elizabeth Gjoneska of the Tsai Lab and Andreas Pfenning from the Kellis Lab, who had met at a seminar on campus. With similarly overlapping interests in how gene regulation, and specifically epigenomic differences, affect the workings and health of the brain, they and other members of the two labs kindled dialogues that soon brought the professors together.
“The collaboration kind of happened organically,” said Kellis, professor of computer science and head of MIT’s Computational Biology Group. “We found kindred spirits – folks who thought similarly but were extremely complementary in their expertise.”
Within two years, the labs had jointly published two major papers. One in Nature, part of a sweeping set of reports on epigenomics that Kellis helped lead, showed that highly analogous sets of gene misregulation signals in the hippocampus of mice and humans each revealed a strong role for the brain’s immune cells and processes in allowing Alzheimer’s disease to progress. The other paper, in Cell, showed that in order to rapidly express genes critical for experience to affect synaptic connections, neurons naturally employ double-strand breaks of their DNA. The team hypothesized that failure to repair these breaks increases with age and may also contribute to neurodegeneration.
Each paper demonstrated the power of their combined approach. Since then, the collaboration has grown significantly to encompass about half a dozen projects. In 2016, for instance, they earned a National Institutes of Health grant to determine the significant epigenomic differences afoot in major brain cell types in Alzheimer’s disease.
In the last year, Kellis and Tsai received an influx of several new NIH grants and philanthropic gifts, such as the one establishing the Alana Down Syndrome Center, enabling them to substantially expand their efforts in Alzheimer’s, tackle new disorders, bring in new collaborators, include new types of experiments, and expand their mechanistic studies. Their new directions include Schizophrenia, Bipolar Disorder, Psychosis in Alzheimer’s Disease, Frontotemporal Dementia, Lewy Body Dementia, and healthy aging.
Importantly, each experiment is designed together, Kellis says. Knowing that the team combines the capabilities of each lab, the team can be more ambitious.
“We think in a different way than any one lab would think by itself,” Kellis said. “For instance, I wouldn’t have the guts to ask many of these things that we are asking, if it wasn’t for our close collaboration with Li-Huei’s lab.”
In the Alana Center, they will apply their team science approach to modeling and analyzing Down syndrome, looking to identify and dissect the unique genetic and molecular signals that explain how the presence of an extra chromosome 21 affects the brain.
And with the new NIH grants, they will ask a litany of questions such as why many people with Alzheimer’s develop psychotic symptoms as well, what are the unique molecular signatures that distinguish Alzheimer’s and other dementias, and how do specific genetic variations in non-coding DNA elevate risk for a number of neurodegenerative and neuropsychiatric disorders.
“How privileged I feel to work with the world’s best computational team,” Tsai said. “This is only possible at MIT.”
Alana Gift to MIT Launches Down Syndrome Research Center

As part of MIT’s continued mission to help build a better world, the Institute announced the creation of the Alana Down Syndrome Center, an innovative new research endeavor, technology development initiative, and fellowship program launched with a $28.6 million gift from Alana Foundation, a nonprofit organization started by Ana Lucia Villela of São Paulo, Brazil.
In addition to multidisciplinary research across neuroscience, biology, engineering, and computer science labs, the gift will fund a four-year program with MIT’s Deshpande Center for Technological Innovation called “Technology to Improve Ability,” in which creative minds around MIT will be encouraged and supported in designing and developing technologies that can improve life for people with different intellectual abilities or other challenges.
The Alana Down Syndrome Center, hosted out of MIT’s Picower Institute for Learning and Memory, will engage the expertise of scientists and engineers in a research effort to increase understanding of the biology and neuroscience of Down syndrome. The center will also provide new training and educational opportunities for early career scientists and students to become involved in Down syndrome research. Together, the center and technology program will work to accelerate the generation, development, and clinical testing of novel interventions and technologies to improve the quality of life for people with Down syndrome.
“At MIT, we value frontier research, particularly when it is aimed at making a better world,” says MIT President L. Rafael Reif. “The Alana Foundation’s inspiring gift will position MIT’s researchers to investigate new pathways to enhance and extend the lives of those with Down syndrome. We are grateful to the Foundation’s leadership — President Ana Lucia Villela and Co-President Marcos Nisti — for entrusting our community with this critical challenge.”
With a $1.7 million gift to MIT in 2015, Alana funded studies to create new laboratory models of Down syndrome and to improve understanding of the mechanisms of the disorder and potential therapies. In creating the new center, MIT and the Alana Foundation officials said they are building on that partnership to promote discovery and technology development aimed at helping people with different abilities gain greater social and practical skills to enhance their participation in the educational system, in the workforce, and in community life.
“We couldn’t be happier and more hopeful as to the size of the impact this Center can generate,” Villela said. “It’s an innovative approach that doesn’t focus on the disability but, instead, focuses on the barriers that can prevent people with Down Syndrome from thriving in life in their own way.”
Marcos Nisti, CEO & Vice-President of Alana, added, “This gift represents all the trust we have in MIT especially because the values our family hold are so aligned with MIT’s own values and its mission.”
Villela and Nisti have two daughters, one with Down syndrome. MIT Executive Vice President and Treasurer Israel Ruiz has had a personal connection to the Foundation.
“It is an extraordinary day,” Ruiz said. “It has been a pleasure getting to know Ana Lucia, Marcos and their family over the past few years. Their work to advance the needs of the Down Syndrome community is truly exemplary, and I look forward to future collaborations. Today, MIT celebrates their generosity in recognizing all abilities and working to provide opportunities to all.”
Down syndrome, also known as trisomy 21, is characterized by extra genetic material from some or all of chromosome 21 in many or all of an individual’s cells and occurs in one out of every 700 babies in the United States. Though the chromosomal hallmark of Down syndrome has been well known for decades, and advances in research, health care and social services have doubled lifespans over the past 25 years, significant challenges remain for individuals with different abilities and their families because the underlying neurobiology of the disorder is complex.
The center will be co-directed by Angelika Amon, the Kathleen and Curtis Marble Professor in Cancer Research, and Li-Huei Tsai, the Picower Professor of Neuroscience. Amon is an expert in understanding the health impacts of chromosomal instability and aneuploidy, the presence of an abnormal chromosome number, while Tsai is renowned for her work in the field of neurodegenerative disorders, including Alzheimer’s disease, which shares important underlying similarities with Down syndrome. In the first four years, the new center will employ cutting-edge techniques to study Down syndrome in the brain with two main focuses: systems and circuits as well as genes and cells.
With the support of the previous Alana Foundation gift, Hiruy Meharena, senior fellow in Tsai’s neuroscience lab, has already been deeply engaged in studying Down syndrome’s impact in the brain at the cellular and genomic level, examining key differences in gene expression in cultures of neurons and glia created from patient-derived induced pluripotent stem cells.
At the molecular and cellular level, Professor Manolis Kellis, director of MIT’s Computational Biology Group and a leader in big-data integration and analysis of genomic, epigenomic, and gene expression data will collaborate with Tsai for single-cell profiling of brain samples to understand the genes, molecular pathways, and cellular states that play causal roles in cognitive differences in Down syndrome.
At the systems and circuits level, Ed Boyden, the Y. Eva Tan Professor in Neurotechnology will lead efforts to conduct high-resolution 3D brain mapping and will collaborate with Tsai to examine the potential of using her emerging non-invasive, sensory-based therapy for Alzheimer’s in Down syndrome.
Amon’s lab will bring its deep expertise from their study of cancer to the new center. They have made important discoveries about how aneuploidy may undermine overall health, for instance by causing stresses within cells. It is their hope that identifying genetic alterations that suppress the stresses associated with trisomy 21 could lead to the development of therapeutics that improve cell function in individuals with Down syndrome.
To further support these research endeavors and to increase the long-term global pipeline of scientists trained in the study of Down syndrome, the Alana Down Syndrome Center will fund postdoctoral Alana Fellowships and graduate fellowships.
The Alana Center will also convene an annual symposium on Down syndrome research, the first of which is tentatively scheduled for this fall.
The Alana Foundation gift supports the MIT Campaign for a Better World, which was publicly launched in 2016 with a mission to advance MIT’s work in education, research, and innovation to address humanity’s urgent challenges. A joint statement guiding the gift’s purpose is available here.

